Resources
Understanding the AMH Test & Interpreting AMH Test Results
What is AMH?
Anti Mullerian Hormone, commonly referred to as AMH, is a hormone generated by the early-stage egg follicles within a woman’s ovaries. Research shows that AMH levels can provide insight into one’s ovarian reserve when compared to women of similar age groups.
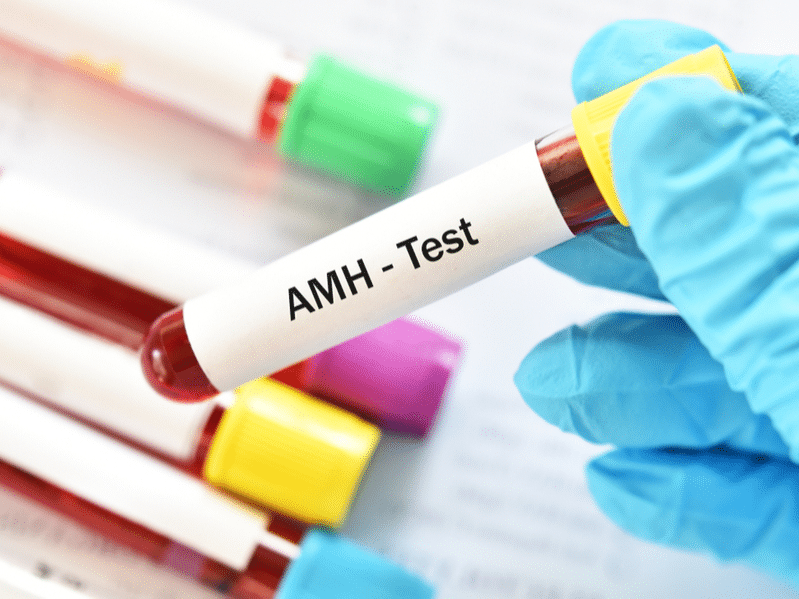
What is an AMH test?
The AMH test is a hormonal blood test that measures the level of Anti Mullerian Hormone in a woman’s blood. This hormone serves as a reliable indicator of ovarian reserve, and the test provides an estimate of the remaining egg count within the ovaries.
How do I get an AMH test?
Anyone seeking further information about their fertility should consult their general practitioner and request a referral to a fertility specialist. Your GP can arrange for an AMH test (along with other tests relevant to fertility) so that your results are available for discussion at your fertility consultation. Results are best interpreted by and discussed with a fertility specialist.
Do I need an AMH test?
The AMH blood test plays a crucial role for those seeking information about their ovarian reserve to assist in family planning. You might consider testing your AMH level if:
• You’ve been actively trying to conceive for more than six months.
• You’re exploring fertility treatments or alternative reproductive options.
• You’ve undergone chemotherapy, ovarian surgery, or any procedures potentially affecting your ovarian reserve.
• There’s a suspicion of an ovarian tumour.
• You desire insights into your remaining eggs and current ovarian reserve.
When should you do an AMH test?
At Fertility North, we advise undergoing an AMH test during the initial days of your menstrual cycle. However, it’s important to note that AMH levels remain stable and are minimally affected by factors such as the menstrual cycle or pregnancy. This means it can be done anytime during your cycle.
For patients at Fertility North, we always communicate and determine the optimal timing with you before your scheduled test date.
Interpreting AMH test results
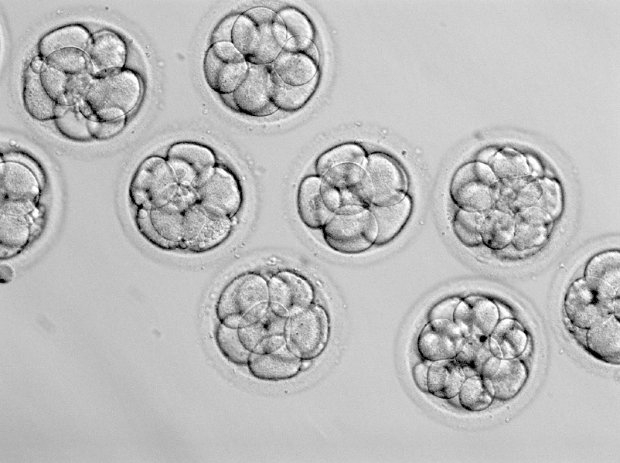
Once the test is completed, your referring doctor will review the results with you. These results can help forecast your response to fertility treatments, providing valuable insights into the procedures that may be most effective. For instance, AMH can predict the anticipated egg count in an IVF cycle, aiding in the planning process. Familiarising yourself with the AMH test and its potential outcomes can empower you to make informed decisions regarding your future fertility plan.
How are the results of the AMH test measured?
The AMH test does not assess egg quality; rather it measures quantity, when combined with ultrasound, this can provide an estimation of the number of eggs expected to develop during a fertility treatment cycle. It is important to interpret the AMH result in context of other factors that influence fertility.
Can AMH levels fluctuate month to month?
Although AMH levels generally offer a reliable estimate of ovarian reserve, there may be minor fluctuations from month to month. However, these variations are typically insignificant and do not significantly impact the interpretation of the results.
What does it mean to have low AMH levels?
Low levels of AMH indicate a diminished ovarian reserve, implying fewer eggs remaining in the ovaries.
Individuals with ovaries are born with the entirety of the eggs they will ever ovulate in their lifetime. The initial egg count can vary significantly among individuals, but regardless of the starting number, the ovarian reserve—meaning the remaining eggs—declines over time. In essence, a lower AMH level corresponds to a decreased number of eggs left in the ovarian reserve. However, it’s important to note that a low AMH level on its own may not necessarily be a cause for concern.
How quickly do AMH levels decrease?
AMH levels typically decrease with age. Although the rate of decline can vary from person to person, a notable decrease is often observed as women reach their late 30s and early 40s.
Factors that influence low AMH Levels & Ovarian Reserve
The primary factors influencing AMH levels and ovarian reserve include polycystic ovary syndrome (PCOS), a history of ovarian surgery, exposure to chemotherapy and other gonadotoxic treatments, obesity, Vitamin D deficiency, and mutations of the BRCA genes. These factors can significantly impact AMH levels and consequently affect ovarian reserve.
Recommendations if you have a low AMH test result
If you receive a low AMH test result, it’s important to discuss the implications and potential next steps with your fertility specialist.
If you are planning to conceive and receive a lower AMH result, you should consider trying for pregnancy sooner rather than later. A low AMH doesn’t mean that you cannot conceive naturally, but it may mean conception may take longer; if you haven’t conceived within six months it is worth seeking specialist advice.
If you aren’t ready to conceive or aren’t sure about what is best, egg freezing may be a good option for those with a diminishing ovarian reserve.
If you are single and want to start a family, we have donor sperm options available.
Normal AMH levels
The reference range, or normal range, for AMH is 5.5 – 37.4pmol/L.
What does it mean to have high AMH levels?
An AMH of >22pmol/L may be associated with PCOS and an increased risk of developing ovarian hyperstimulation syndrome (OHSS), an over-response to the stimulation medications used in fertility treatments.
If you have a high AMH result, your doctor will discuss what this means with you and work with you to devise a pathway forward and create a treatment plan that is tailored to your individual results should you choose to embark on treatment.
Are AMH tests reliable?
AMH tests are widely regarded as reliable and accurate tools for evaluating a woman’s ovarian reserve. However, it’s important to note that a high intake of biotin (Vitamin B7) could potentially affect the accuracy of the results.
When combined with specialised ultrasound assessing small follicles in each ovary, the AMH test provides a comprehensive view of potential future fertility.
Why is the AMH test important?
The primary advantage of undergoing an AMH test lies in its ability to provide foresight. Given the increasing average age of women when starting families, many specialists emphasise the importance of considering reproductive options earlier rather than later. Conditions like polycystic ovary syndrome (PCOS) can impact fertility, making understanding your AMH level crucial. Being aware of whether you have normal AMH levels can significantly inform your reproductive decisions. For example, individuals with lower AMH levels might opt to research and explore fertility preservation or treatment options at an earlier stage. This proactive approach can empower individuals to make informed choices about their reproductive health and future.
It is important to note that AMH results are not fully indicative of your fertility capabilities, it is just one of many investigative tests used to aid in the diagnosis of infertility.