Advanced Technology
Preimplantation Genetic Testing
A range of cutting-edge techniques used to test the genetic and chromosomal makeup of embryos.
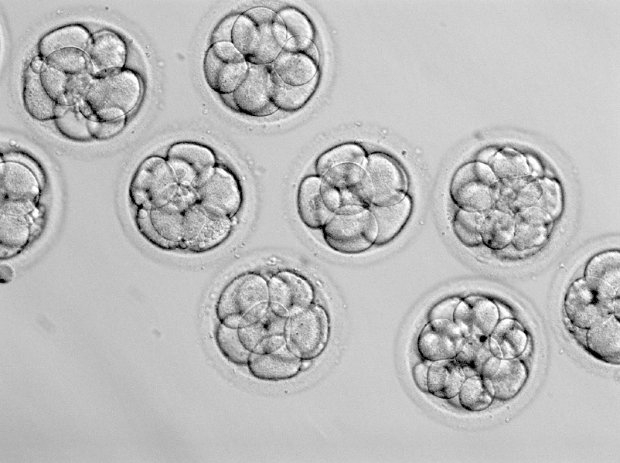
Most cycles of IVF or ICSI result in the creation of more than one embryo. The best embryo is usually selected for transfer based on its rate and pattern of cell division, as well as its appearance. Unfortunately though, these are not an accurate measure of whether an embryo is genetically normal or ‘Euploid’. Embryos that are not genetically normal are known as aneuploid, and they may have lost or gained genetic material along the way – genes (tiny pieces of genetic coding) or whole chromosomes.
Because human reproduction is inherently flawed, at least 50% of human embryos are aneuploid. While some genetic abnormalities are compatible with life, most will result in either failure of the embryo to develop, implant, or culminate in a healthy, live birth. As such, embryo aneuploidy can be responsible for recurrent implantation failure (multiple embryo transfers with no success), and is the primary cause of miscarriage and early pregnancy loss.
What is Preimplantation Genetic Testing (PGT)?
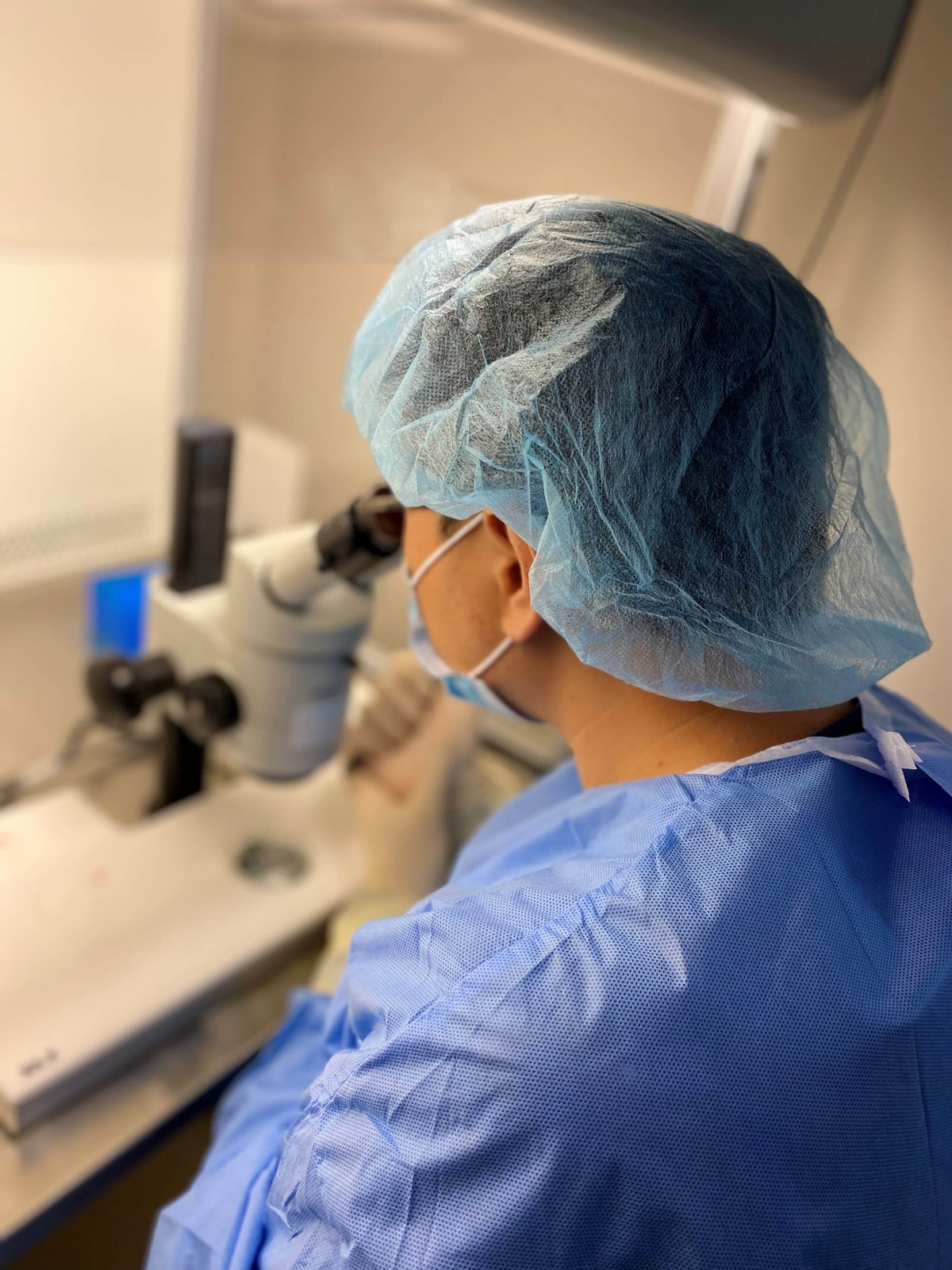
Pre-implantation Genetic Testing, or PGT, is a highly specialised laboratory procedure that enables us to check an embryo for chromosomal and genetic abnormalities.
PGT enables us to identify the genetically normal embryos to use for treatment.
There are three different types of PGT:
PGT-A
PGT for Aneuploidy is used to check that the embryo has a normal number of chromosomes. Sometimes, the cells in an embryo can gain an extra copy of a chromosome (trisomy), lose a copy (monosomy) or have more complicated rearrangements, gains or losses. These embryos are abnormal and are known to be ‘Aneuploid’.
The most recognised example of aneuploidy is an extra copy of chromosome 21 (trisomy 21), more commonly known as Down Syndrome. Embryo aneuploidy can be responsible for recurrent implantation failure (multiple embryo transfers with no success), and is the primary cause of miscarriage and early pregnancy loss.
PGT-M
PGT for Monogenic / Single Gene Disorders is used to test embryos for genetic abnormalities involving a single human gene and/or when a segment of one chromosome is transferred to another chromosome. A common example of these includes the breast cancer genes BRAC1 or BRAC2, or changes in the HTT gene, causing Huntington’s Disease. Other single gene disorders include Thalassaemia, Cystic Fibrosis, Haemophilia, Spinal Muscular Atrophy and Fragile X Syndrome.
PGT-SR
PGT for Chromosomal Structural Rearrangements is utilised to identify embryos in which the structure of a chromosome has been altered – this can result in missing or extra genetic information in the embryo which may result in failed embryo development, failed embryo implantation or a higher chance of miscarriage.
What are the risks of PGT?
The embryo biopsy procedure itself is considered safe and is not known to be associated with any increase in birth defects when compared with children born following fertility treatment without embryo biopsy.
PGT is not capable of testing for non-genetic, congenital birth formations, such as Spina Bifida or cleft lip/palate.
Who is PGT suitable for?
The use of Preimplantation Genetic Testing in Western Australia is regulated by law, so it can only be used in specific instances.
PGT may be recommended by your doctor if you:
- Are known to carry a genetic or chromosomal condition.
- Are of advanced maternal age (> 35 years).
- Have had repeated, unsuccessful attempts with IVF, ICSI and / or FET.
- Have experienced recurrent miscarriage.